A Look at Behavioral Health

Pediatric behavioral healthcare (BH) is an umbrella term for the care of children with a range of emotional, psychiatric, or behavioral conditions or illnesses. This includes diagnoses that fall under the mental health category. Examples can include anxiety, ADHD, depression, addiction, and PTSD.
Integrated behavioral healthcare (IBHC) is the goal of a pediatric office to coordinate care seamlessly with the patient, family, and other healthcare + providers to care for the health of the patient’s body and mind.
Existing Research on ACEs
Adverse Childhood Experiences (ACEs) have been found in at least one major study by the CDC to directly affect physical and emotional health of children and adolescents. The CDC-Kaiser study2 concluded that a variety of factors, including environment, parental mental illness, poverty, abuse, and neglect contribute to these debilitating effects, leading to ill health, increase in risky behaviors, and maladaptive patterns through generations.
ACEs occur by nomenclature in childhood, so early intervention is key. The role of pediatric providers is crucial in both the prevention and treatment of childhood traumas, as well as in the coordination of care between pediatrician and pediatric behavioral health professionals. The culture of integrated medicine is leading many pediatricians to believe that they are part of a healthcare team responsible not only for the physical well-being of their patients, but their emotional and mental health too.
Benefits of BHI in the Patient Centered Medical Home
The Patient Centered Medical Home (PCMH) is an important tenet in the integration of behavioral healthcare. Beyond the occasional financial benefits for the practice from payors and recognition by NCQA, there are enormous benefits to patients.
Early intervention is key in the long term treatment of pediatric BH. The important relationship of trust between a patient and their PCMH enables the practice to mark changes and diagnose BH concerns early. By diagnosing, treating, and referring BH to a professional such as a pediatric psychologist, the patient and family are guided to valuable resources early, from a relationship they trust.
Finally, BHI offers pediatric practices the opportunity to offer a whole-person, or integrative, healthcare perspective, that cares for the patient’s mind, body, and wellbeing. This leads to overall better outcomes for the patient.
Aims for this Guide
This e-guide aims to inform and provide resources for independent pediatricians as they integrate behavioral healthcare into their practice and workflows.
The Business Case for Behavioral Health Integration
You can never be positive that any business decision will be a success, but you can make the wisest decision by studying the business case for that decision in all its permutations beforehand.
For behavioral health integration, this translates to the following:
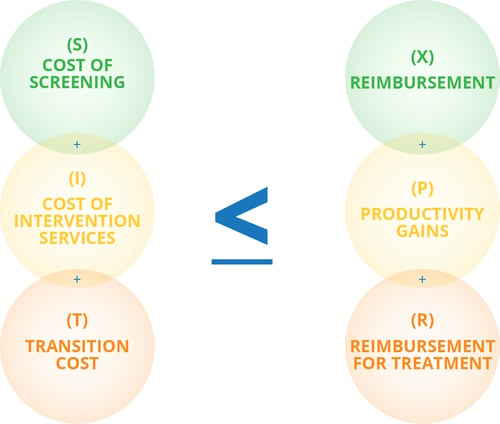
For example, a practice already offers screenings for depression, anxiety, and certain behavioral issues for its patients. The assumed additional cost of screenings is, therefore, $0. The practice would like to integrate further BH services and seeks to hire a full-time pediatric psychologist.
The transition costs include repairs to the new employee’s office (~$1000 to $10,000 depending on the state of the room), as well as marketing efforts ($200-$300 for job boards, newspapers, and social media ads), the time to interview and hire a candidate (10-20 hours), and finally the additional insurance, benefits, and pay for the employee, which can range from $45k a year to over $100k in large cities. If the new staff member doesn’t bring a client base with them, the practice will need to fill the gap with appropriate care for their existing patients, or will likely need to absorb the costs of a small beginning clientele.
If the practice can earn enough revenue to cover all these startup and ongoing costs through their reimbursement for screenings, referrals to in-house care, and gains in productivity thanks to behavioral healthcare workflows being taken over by one dedicated employee, they can feasibly make the change. If they cannot, the practice should refer to other options, which this guide will discuss shortly.

In essence, this formula is designed to keep costs below revenue, to make BHI beneficial for the practice as a business, which makes it convenient and long-standing for patients.
Business cases will vary based on your individual practice’s resources, needs, and workflows. Screenings might be given during the visit, meaning a shorter visit time, or they might be given online, saving time and revenue. Intervention services range from large investments to none at all, and reimbursement is different for each state and provider.
The following chapters will guide you through the options of integrating behavioral health into an independent pediatric practice, so that you can choose the integration methods and services that best work for your practice’s budget and your patient’s needs.
IBHC Spectrum
There is no single, “correct” way to integrate behavioral health into pediatric healthcare, partly because no two offices are alike, and partly because qualifications of specialists and the needs of communities -- and the resources of practices -- differ. Below are the most common options for BHI, with their pros and cons for offices. Keep in mind that combining methods may work best for your office.
The first three methods explored below -- consultation, telemedicine, and resource-based care--- are low-impact ways of integrating BH into your practice, without significant change to budgets, workflows, or revenues. The last two-- coordination and colocation -- are larger, structural changes that integrate BH professionals into workflows, teams, and your office space.
Expect structural BHI changes to take time. One group practice in Michigan reports that successful integration can last from at least 6 months to 5 years. Like any major business decision, the changes set in place should be evaluated for success and methods of improvement, including by financial records, and formal or informal patient and staff surveys.
Consultation
Consultation allows the pediatrician to speak to a BH specialist, such as a psychologist, in a professional context about the needs of a specific patient. The pediatrician in this case is the referring provider, and the psychologist the advising provider. Upon review of the patient’s case with the pediatrician, the psychologist may recommend treatment and care for symptoms or offer a diagnosis.
The psychologist or other specialist doesn’t need to see the patient for a consultation to be successful. After a consult, the pediatrician may be satisfied that they are providing adequate care for a child’s diagnosis. If deemed necessary, the consult can result in a referral of the child to the psychologist for an initial visit, to see if long-term care is more appropriate for their health and well-being. Long-term care would then be coordinated by both providers. See the below section on coordination of care.
Telemedicine
If you conduct telemedicine and bill for it at your practice, it may be more convenient to set up telemedicine visits specifically for BH patients who will require many visits over time -- for example, patients with well-managed ADHD or a behavioral disorder who require a visit prior to authorization for controlled substances. A faster, more convenient option for families and providers might be to schedule the visit via phone or Skype between regular well visits at the office, making telemedicine an ideal convenience for practices and families.

Resource-based Care
Resources for practices vary hugely. If budgets are tight or your practice is simply not in a position to integrate BH into existing workflows right now, there are still methods you can employ to educate patients and lead them to obtaining appropriate care. Regular behavioral and mental health screenings, meaning at every well visit, can help detect problems and lead patients to early intervention and resources. In addition, a strong referral network is equally the best way for resource-strapped practices to make sure their patients are receiving the care they need. Keep in mind the hurdles that caregivers have to navigate to give their child access to referred appointments. These include but are not limited to travel time, transportation, and scheduling.
Coordination
Coordinating BH involves a professional connection between two professionals -- the pediatrician and the BH specialist (psychologist, counselor, psychiatrist, or other). In multiple-provider offices, the offices may coordinate as two groups.
Coordination of care is an important part of any health system, but in this definition, involves a more direct relationship between professionals which is nonetheless specific to circumstances.
Colocation
Colocation and coordination overlap in that a BH specialist may choose to host office hours in a pediatric practice only part of the time.
For the most part, however, colocation is perhaps the largest business commitment to BHI, because it combines the services of pediatrician and BH specialist together as official or unofficial business partners. The colocation of another provider implies that this provider will have access to your EHR, patient records, workflows, schedules, and also be a part of the payroll. However, the arrangement could suit completely separate offices who simply share the space, whether because there is a surplus of room, or because the two offices have opposite office hours.
Colocation is arguably the most convenient way for patients to access integrated care, as more of their needs are being met within the same space. On the flip side, for most independent practices, this decision requires the most upheaval to office space, workflows, and office dynamics.
Success In Integration
To successfully integrate BH, you must first determine that the addition of services or resources is reasonable and practical for your practice. Not every office can bring a psychologist on staff, but every office can offer outside resources, guidance, and support for patients as they navigate their behavioral health. Your practice may also find it useful to create a 5-year plan for integrating behavioral health to meet your goals
Telemedicine
Because behavioral health diagnoses can be difficult for the patient to describe, especially if they are very young, it’s important to maintain a positive, consistent relationship with one or more parents or caregivers in order to communicate effectively with families about behavioral health. This is especially important for telemedicine visits between physical visits -- there is no reason the same care can’t be offered at both.
First, assess your existing workflows. If your practice has telemedicine procedures set up already, determine if there are or can be visit types for behavioral health. Telemedicine is a great resource for families without reliable transportation, or for patients who require many visits over a long period, such as patients with ADD/ADHD.
If your practice does not offer telemedicine services, your first step should be to determine the reason and necessity for introducing telemedicine into your practice. It is likely not financially feasible to introduce telemedicine only for behavioral health visits, however many kinds of visits may benefit from the service, such as follow up visits and after hours visits. Secondly, determine how you will be paid for telemedicine -- this will involve a conversation with your payors and a discussion with billers to code telehealth visits appropriately.

The Center for Medicaid and Medicare Services (CMS.gov) offers resources for billing and coding telemedicine visits, as well as information about telemedicine in health professional shortage areas. Remember to bill telemedicine in addition to correct codes, such as for after hours visits (99050) or an emergency requiring a visit outside the office (99060).
Finally, once you’ve started offering telemedicine at your practice, be sure patients know about it. The added convenience can introduce visits for patients they may otherwise have missed, or which would have caused them to miss school and caregivers to miss work. Marketing efforts don’t need to be extravagant, and can find much success on your practice’s website or social media accounts. Over time, as patients find the service convenient or helpful, they are likely to recommend it to other families.
Optional: Telehealth Tech
The only tools truly necessary for telemedicine are a laptop or smartphone, and these are also the most common tools used in telemedicine visits. If you’re considering an upgrade to more specialized equipment such as cameras or microphones for your telemedicine visits, be sure that telemedicine is a consistent choice for your patients.
Here's some tech that can elevate your telemedicine visits:
Consultation
As a medical professional, you may have sometimes or often felt at a loss for how to treat or prescribe methods of care for a patient with a behavioral issue. Time may also be a concern -- when an adolescent expresses suicidal ideations, your first instinct as a provider is to give the patient the time necessary to identify immediate risks and symptoms, as well as to provide care. With occurrences of childhood mental illness on the rise, however, it can be difficult to afford the time necessary to BH patients.
Pediatricians are experts at what they do. The aim of this guide is not to outline when a patient should see a specialist or be referred for regular treatment, but to offer the resources to offer patients and providers the peace of mind of coordinated BH.
Locating Consulting Providers
Here are some steps to connect with behavioral health specialists to consult or to refer your patients to:
1. Check your state’s resources to see if there are programs or processes to contact BH specialists near you. You might get a new contact or even ways to help your patients afford copays with their new provider.
2. Invite a prime candidate or two out for lunch and see if your expectations are the same. Can they provide the best care for your patients?
3. Do they accept referrals from other practices and can they handle both loads?
4. Establish a protocol for consultation services, including what constitutes a timely response via phone or email, and protocols for referring services. Gather as much information as possible to counsel families on what to expect.
The methods of an actual consultation depend on the two providers’ professional relationship and the patient’s needs -- remember to ask questions, clarify ideas, and establish an agreed course of action before ending the discussion.
Coordination
Some coordination is involved in communicating the needs of a patient two providers independently offer, however, as most practices already practice this professional courtesy, in this guide, coordination refers to the regular, cyclical exchange of resources between pediatrician and BH specialist, in order to provide the best care for patients.
To coordinate with another provider, you do not need to have an existing relationship with them, but a positive impression never hurts. The simplest way to coordinate with another provider is simply to ask, and then take steps as deemed appropriate. To make a coordinated agreement work between both offices, here are some things to consider:
- Shared locale or building--can your patients access the BH specialist upstairs or across town?
- Alignment of office hours
- Designated workflows (e.g., a youth who screens positive for depression or anxiety is automatically referred to the BH specialist for an initial consult)
- Written agreement of practices and protocol between the two offices, including communication preferences
- Ability of front desk stagg to cover one another's shifts
- Transparency of coordinated efforts to families
- Culture and leadership styles (e.g., disciplining a late employee or negotiating payment plans with families)

REMEMBER
State laws stricter than HIPAA take precedence. Be sure to know your state's PHI laws thoroughly and communicate medical information only when necessary to the wellbeing of the patient.
Coordination via Colocation
While many offices share a professional coordinating relationship that benefits patients of both offices, some practices may choose to also share a physical location with a BH specialist, whether that’s an extra room or the whole office for certain days and times.
Colocating with another office does not necessarily mean the offices must exchange records or share other resources, however, care should be taken to preserve the privacy of data and other sensitive resources, such as notes, sample medications, and vaccines between offices.
Colocation
Combining offices, resources, and income with another provider is a huge step forward in a pediatric practice’s history as a small business, and as with any addition to the team, cause for celebration. To help get you started and mitigate risks, here’s how to make your new team the pinnacle of integrated care.
Respect and Communication
What’s good for the first-graders in your care is good for your practice too. Any partnership is bound to run into miscommunication and hard feelings eventually -- successful relationships are all about how you bounce back.
Respect boundaries and your partner’s unique style of care. If your partner counselor can’t be available after 3pm because she has to be home for her kids, make that clear to your patients before referral. If you get criticism from families about your BH provider, try to walk the balance between listening to concerns and defending your colleague.
Make Priorities Clear
Whether your new colleague is a partner or employee, make sure your values for patient care align and priorities are made clear. Occasionally, the patient's emotional or physical health may take priority, and both providers are responsible for acting on behalf of the best interest of the patient at the moment.
-
- Case Study A: You're a nurse practitioner, and during flu season, you ask your BH partner to send in mutual patients after their sessions to discuss and receive the flu vaccine. You might like the idea of efficient flu visits, but let the BH provider give the green light so young patients aren't given a new stressful experience after a difficult session.
- Case Study B: You're a pediatric psychologist, and one of your most difficult adolescent cases has been making steady progress in battling his depression. During your conversation you discover he may be at risk for an STD. It might be important to continue to make therapeutic progress, but it's also a good time to consult with your pediatrician to schedule the patient for a urinanalysis test and counsel on protective practices.
- Case Study A: You're a nurse practitioner, and during flu season, you ask your BH partner to send in mutual patients after their sessions to discuss and receive the flu vaccine. You might like the idea of efficient flu visits, but let the BH provider give the green light so young patients aren't given a new stressful experience after a difficult session.
Make it Official
Your new colleague should have designated office space and resources, including but not limited to front desk staff and medical records. Make the sharing official with a signed lease or partnership agreement. Legal agreements protect everyone and make difficulties down the road easier to navigate. Remember to consult a lawyer for legal device.
Know When to Quit
Not all relationships work out. If your values, patients' needs, or care styles change over time or don't match well despite repeated tries, it may be better for your patients to continue to see their BH specialist and pediatrician separately.
In some cases, you may ask your colleague to leave, and will be able to promote or hire another to take their place. In others, you may be the one to relocate.
Separating from a professional partner isn't a sign of failure, but a step forward in creating a better integrative system for both of your patients.
Grow Together
Whether you decide to take on a BH specialist as an employee or partner, if you're moving from a single provider practice to a multi-provider office, it's necessary to get some business affairs in order.
If you're marketing a business under your own name, consider legal options, such as rebranding as an LLC with the advice of a lawyer. This is the next step up from simply sharing office space and patients and growing a business with your new partner. If the partner is an employee, you'll have to register for an Employee Identification Number. If they're coming on as a partner, consult an accountant for the correct forms to file, such as the "US Return of Partnership Income," and individual K-1s.
A Professional Care Team
You already know how to manage a team, whether it’s you and a front desk person or you are one of several providers in a group practice. Whether the specialist you choose to assist your patients is on-site or off, it bodes well to consider them a part of the team. After all, the moment they take on your patient as their own, you are both fighting the same battles -- against disease and illness, and for wellness and positive growth.
Whether you choose to practice together or over the phone, via referral or regular team meetings, embrace your new team member as you would a new employee, even if your practices are separate. Understand their values and beliefs, question them about common prescriptions and the length of treatments. Share your methods of addressing family concerns or complex patients -- not only will a BH specialist appreciate insider information on their new patient, but by working together, the two of you can also ensure that wherever your patients go, they are treated with compassionate care that is familiar and trustworthy.
Conclusion: How to Find the BH Specialist for Your Practice
A psychologist, counselor, or therapist isn’t going to appear out of thin air to fulfill your dreams of integrated emotional and behavioral care for your patients. Recognizing the need for help is the first step towards that goal. Not sure where to begin? Here’s our list:
1. Determine needs. Get specific and detail how your patients could use a BH specialist. Do they need specialized psychiatric medication? A psychiatrist could help. Do they need tools to do better in school and at home? A counselor or family therapist could work with parents as well as children.
2. Determine logistics, such as cost and space. Your practice may have the space but not the income to support a full time BH provider. Consider a part time provider or one who can employ students to volunteer in exchange for credit hours.
3. Connect with your network. Not just your colleagues and friends in pediatrics, but state officials, your existing staff, and your patients. Ideas, advice, and referrals can come from anywhere, and you can address any concerns at the outset.
4. Start small. If welcoming a BH provider into the room next door seems a little too overwhelming or expensive, start small by cultivating relationships with local professionals and referring patients. If you’re a larger, long standing practice, consider the benefits of hiring or consulting with a professional who can offer lower costs. If you’re starting a practice from scratch, you may find success in setting up with a BH provider who aims for retirement in a few years and can educate you on the community and perhaps offer office space.
5. Write a business plan. When your ideas for BHI are nearly fully formed, write them down into an agreement or a business plan. This will help you solidify your goals for integrating behavioral health, as well as prepare you for setbacks and create reasonable goals.
If you plan to take the steps to integrate BH into your practice’s workflows, congratulations. Integrative healthcare is a win for practice and patients, and while access to healthcare continues to be a concern, your work as a pediatrician can help close the gap.
Small steps to integrate care allow children access to the care they need from the medical home they trust you to provide.